Introduction:
Despite progress made in the treatment of multiple myeloma (MM), a significant percentage of patients are unable to receive second line of therapy. Our study evaluated the burden of infectious complications, and other factors that may play a role in hindering patients from receiving subsequent lines of therapy at a comprehensive teaching hospital.
Methods:
Patients with MM treated between 2014 and 2019 at Rochester General Hospital were selected from the MM registry. Tool was designed on REDCap for retrospective data collection from electronic medical records. Patients who declined therapy, never received treatment, had smoldering myeloma, or with a concomitant immunocompromising state were excluded. Out of 159 patients, 119 were eligible for analysis. We studied the relationship between patient demographics, clinical characteristics, treatment regimens, and outcomes. Binary logistic regression was used to determine which factors were significant in determining advancement in the line of treatment. The chi-squared statistic was used to determine significance with a Type I error rate set at 0.05.
Results:
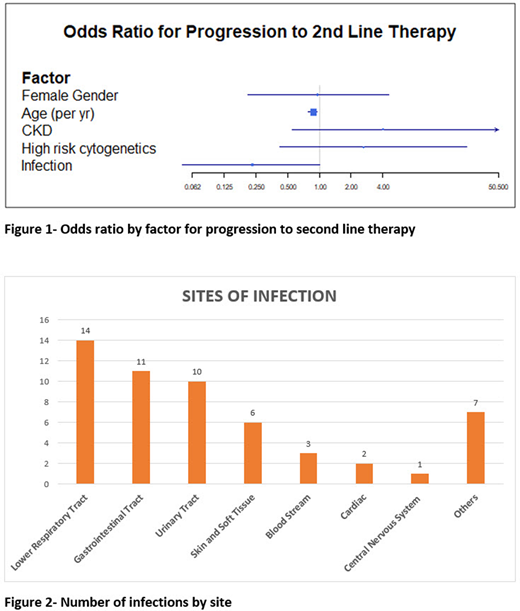
The median age at diagnosis of MM was 68.5 years (Interquartile range=59.2-76.9), 55.4% (n=66) were males, 72.3% (n=86) were Caucasian. Revised International Staging System (R-ISS) staging was available for 77 patients, 27.3% (n=21) were stage I, 58.4% (n=45) were stage II, and 14.3% (n=11) were stage III. Cytogenetics were available for 93 patients, 76.3% (n=71) were standard risk and 23.7% (n=22) were high risk [17p del, t(4;14) or t(4;16)]. A three-drug induction regimen was administered to 61.3% (n=73) patients. Autologous stem cell transplant was performed in 39.5 % (n=47). Sixty-seven patients (56.3 %) received second line therapy. Twenty-six patients did not have a relapse after the first line at the time of data censorship. Patients who did not receive a second line treatment after relapse or progression were 21.8% (n=26). The factors prohibiting proceeding to a second line regimen (can be multiple) included patient preference/poor performance status (n=15), death while on first line treatment (n=15), advanced age (n=6) and prohibitive co-morbidity (n=4). Binary logistic regression showed age to be a significant negative predictor for receiving second line therapy. The odds ratio (OR) of receiving second line therapy was 0.88 for every year increase in age, 95% CI (0.78-0.95), p=0.007 (Figure 1). One or more documented infections within 6 months of diagnosing MM or until transplant date occurred in 32.8% (n=39). Types of infections are depicted in Figure 2. Documented infection was a borderline significant negative predictor for receiving second line therapy with OR =0.23, 95% CI (0.05-1.003), p=0.059. Race, pre-existing chronic kidney disease (CKD), gender and high-risk cytogenetics were not significant predictors of receiving second line therapy (Figure 1).
Conclusion:
Our study identified advancing age as a significant negative predictive factor to receipt of second line therapy in MM. Documented infections, while borderline significant, had a high impact as to whether a patient receives second line therapy. Strategies such as a formalized geriatric assessment, tailored treatment for frail patients, and infection prevention measures might increase odds of receiving second line therapy and may result in improved outcomes.
Jamshed:Takeda, Amgen and Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal